Cervical Artificial Disc Arthroplasty
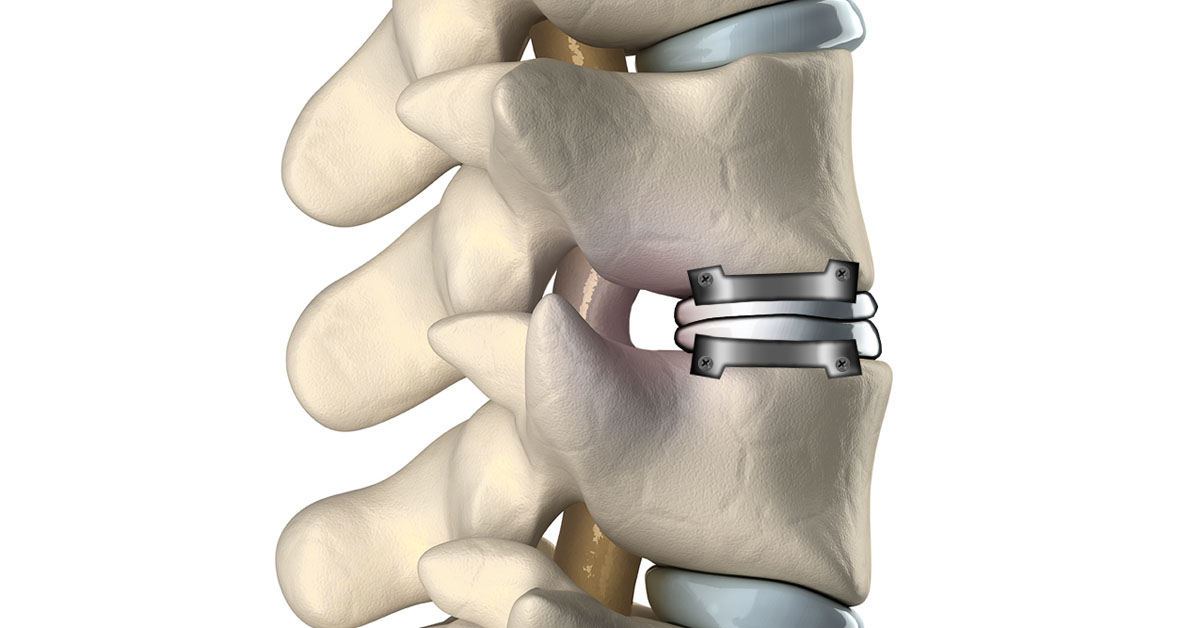
Cervical Artificial Disc Replacement is a procedure which replaces a diseased or damaged disc with a stainless steel device designed to maintain motion. This device has two joining components: a ball on top and a trough on the bottom. It is inserted into the disc space and attached to the vertebral bodies on both sides.
Who needs cervical artificial disc replacement?
This procedure is not recommended for all patients with neck pain or radiculopathy. The physician determines whether a patient needs artificial cervical disc replacement depending on the symptoms, diagnosis and anatomy of neck. Usually this surgery is suggested for patients who have:
- Severe stenosis with spinal cord injury
- Severe facet arthritis
- Cervical kyphosis
- Primary bone pathology such as infection
Procedure
The steps involved in the cervical artificial disc replacement procedure are following.
Incision
The surgeon approaches the neck from the front and makes an incision in the neck. The tissues and blood veins are moved aside to allow for a clear view of the damaged disc and to gain access to the spine.
Disc Removal
The damaged or diseased disc is completely removed from between the vertebrae. The impinging disc fragments or bone spurs are also removed.
Shaping
The disc space is distracted to the usual disc height to relieve stress on the nerve roots. Then the surfaces of the upper and lower vertebrae are cleared of all the damaged disc tissues and shaped to accept the implant.
Implant
With the help of fluoroscopy or X-rays, the device is implanted in the prepared space between two vertebrae. The device is secured with specialized screws. The implant is designed to preserve motions of spine such as flexion, extension, side bending and rotation. It also helps to keep the cervical spine properly aligned.
Closure
The wound is then closed with a few stitches or medical glue. The bandage is applied after cleaning the wound.
After the surgery
The patient is usually discharged from the hospital after 24 to 48 hours of operation. This surgical procedure has minimal movement limitations. The risks of this surgery include early or late loosening of the components, anatomical or technical difficulties, and component sizing issues. Other possible problems include tissue reaction and formation of bone that may reduce spinal motion or result in a fusion.
This material is intended to give the patient an overview of surgical procedures and treatments and is not intended to replace the advice and guidance of a physician. Always consult with your doctor about the particular risks and benefits of your treatment.
